by Paul Wynn
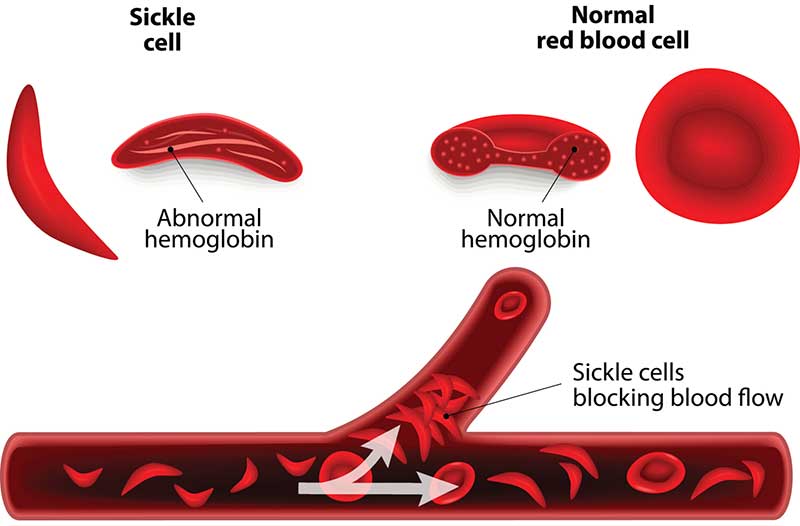
When round and smooth, red blood cells move easily through the body carrying oxygen from the lungs to vital organs. In sickle cell disease, red blood cells are shaped like sickles or crescent moons. These stiff, sticky cells catch on to each other and stick to the walls of the blood vessels. The cells get stuck blocking blood flow and oxygen.
Parts of the body – like the heart, lungs and kidneys – that don’t receive normal blood flow eventually become damaged. This leads to other health complications like anemia, pain and inflammation and stroke.
“There are no medicines that cure sickle cell disease, but treatments may relieve pain, prevent complications and help people live longer,” says Dr. Lewis Hsu, chief medical officer of the Sickle Cell Disease Association of America and director of pediatric sickle cell at the University of Illinois in Chicago.
How Do You Get Sickle Cell Disease?
Sickle cell disease is a hereditary condition passed on by parents, much like hair color and eye color. It’s not contagious like a virus.
People with sickle cell disease carry two genes from both parents of altered hemoglobin, a protein that allows red blood cells to carry oxygen to all parts of the body. Some individuals carry the sickle cell trait because they only have one mutated gene.
If one parent has sickle cell disease and the other carries the sickle cell trait, there’s a 50% chance of giving birth to a baby with either sickle cell disease or sickle cell traits. When both parents have a sickle cell trait they have a 25% chance of having a baby with sickle cell disease. Sickle cell disease is a recessive condition because you need to inherit a mutated gene from each parent to develop it.
The median life expectancy of people with sickle cell disease is between 42- and 47-years-old, according to the American Society of Hematology. “The life span has definitely improved since the 70s when most people didn’t make it to adulthood, but we still have a long way to go to improve longevity,” says Dr. Enrico Novelli, medical director of the UPMC Adult Sickle Cell Disease Program in Pittsburgh.

Sickle cell disease is the most common inherited condition in the world, affecting 8 to 12 million people. It mainly affects families who originate from parts of the globe where malaria is common. These areas include:
Who Gets the Disease?
- Sub-Saharan Africa.
- Middle East.
- Parts of India.
- Caribbean.
- Mediterranean countries like Italy, Greece and Turkey.
Sickle cell disease affects these populations because having the sickle cell trait protects individuals from serious consequences of malaria, according to the Centers for Disease Control and Prevention.
In the United States, it’s considered a rare disease affecting about 100,000 Americans, says the CDC. In addition, the government agency reports that sickle cell disease occurs in about 1 in every 365 Black or African-American births and 1 out of every 16,300 Hispanic births.
Through national newborn screening guidelines implemented in all 50 states and the District of Columbia, babies are tested for sickle cell disease. About 2,000 babies are born with the disease each year in America, according to the American Academy of Pediatrics.
Types of Sickle Cell Disease
Sickle cell disease refers to a group of blood disorders caused by “sickled” hemoglobin. The specific type of sickle cell disease that someone has depends on the kind of hemoglobin, in addition to the inherited gene they receive from their parents.
The most common types of sickle cell disease include:
- Sickle cell anemia: This is the most common and severe form of sickle cell disease. People with this type inherit two sickle cell genes, one from each parent.
- Sickle hemoglobin-C disease: People with sickle hemoglobin-C disease inherit a sickle cell gene (“S”) from one parent and from the other parent a gene for an abnormal hemoglobin called “C”. This is usually a milder form of sickle cell disease. Some people also inherit rarer types of hemoglobin D, E and O. The severity of these rarer types of sickle cell disease varies.
- Hemoglobin S–beta-thalassemia: When individuals are diagnosed with this form of sickle cell disease, they inherit one sickle cell gene from one parent and one gene for beta thalassemia from another parent. Beta thalassemia, a type of anemia, comes in two types: 0 and +. For those with beta-0 thalassemia, their condition is usually more severe, while beta+ thalassemia tends to be a milder case.
Treatment and Care
The main goal of treatment is to reduce painful episodes and prevent symptoms like anemia, swelling of feet and hands, frequent infections and vision problems – tiny blood vessels in the eyes can get stuck with sickle cells and cause retinal damage.
There are several medications that patients can learn about to help manage their complications. “The amount of research has significantly multiplied in the last few decades,” says Hsu. “Within the past five years, there’s been three new treatments approved by the FDA that take unique approaches to treating sickle cell disease.”
The following Food and Drug Administration-approved prescription medicines can help reduce and manage certain complications related to sickle cell disease:
- Hydroxyurea (Droxia, Hydrea, Siklos). Approved by the FDA in 1998, hydroxyurea has been shown in studies to reduce pain-related symptoms of sickle cell disease, the need for blood transfusions and hospitalizations. It does require monitoring for possible side effects, including low blood counts that may predispose one to infections and bleeding.
- L-glutamine oral powder (Endari). This medicine is approved to reduce acute complications of sickle cell disease in patients 5 years of age and older. In studies, this drug was shown to reduce hospitalizations due to pain episodes and shown to increase the time between pain symptoms. This medicine may cause some side effects such as constipation, nausea, headache, pain in stomach area and cough, among others.
- Crizanlizumab (Adakveo). In 2019, the FDA approved this monthly IV biologic medicine to reduce the frequency of a vaso-occlusive crisis, or sickle cell crisis, such as acute episodes of pain. The medicine was approved for patients aged 16 years and older. Side effects may include nausea, joint pain, back pain, fever and infusion reactions.
- Voxelotor (Oxbryta). This oral medicine was approved in 2019 to improve anemia in people with sickle cell disease. Hypersensitivity reactions were the most commonly reported side effect following treatment. Other side effects may include generalized rash, mild shortness of breath and mild facial swelling.
Non-Medication Options
In addition to available medications, there are two approaches that are usually recommended for those with severe cases of sickle cell disease. These options include:
- Blood transfusions. During a blood transfusion, normal red blood cells are added to increase the supply of oxygen to all parts of the body. Blood transfusions are particularly common among those with severe anemia. Sickle cell crisis can lead to kidney damage. anemia related to kidney failure is best treated by replacing the hormone the kidneys are supposed to make (erythropoietin) and not by regular transfusions. Stroke prevention can require monthly transfusions. Exchange transfusions are preferred to avoid iron overload for patients.
- Stem cell transplant. During this procedure, bone marrow is replaced with healthy bone marrow from a donor, usually a sibling who does not live with sickle cell disease. There may be serious complications related to stem cell transplants, and there’s a long recovery period so these procedures are usually reserved for those with severe cases. It’s not surgery. Hsu notes that about 1,700 stem cell transplants have been performed throughout the world.
Survival and Prognosis
The survival of young children diagnosed with sickle cell disease has significantly improved since the 1970s, says Novelli. More than 98% of children with sickle cell disease live to become adults, according to a study published in the journal Blood. Improved survival rates are attributed to national newborn screening, early treatment with penicillin and effective vaccinations against flu and pneumonia.
Children with sickle cell anemia might receive penicillin between the ages of about 2 months old until at least age 5. Doing so helps prevent infections, such as pneumonia, which can be life-threatening to children with sickle cell anemia.
Despite improvements in mortality rates and advancements in sickle cell disease research, there’s still much more progress to be made. Gene therapy may provide hope for a cure in the future. There are a half-dozen gene therapy programs underway that are taking different approaches to either replacing genetic material, removing or correcting cells – called gene editing – or replacing cells with modified ones.
“Gene therapy may offer hope for this patient community that they have been waiting for, but we won’t know until the studies are much further along,” says Hsu.
Copyright 2022 U.S. News & World Report