By C.C. Campbell-Rock
Suppose you scheduled a medical procedure at a hospital. In that case, you have the right to access a listing of hospital prices that allows you to competitively shop for the best prices at various institutions. Even then hospital sticker shock is still a thing.
In 2019, the Center for Medicare and Medicaid Services (CMS) issued a hospital pricing transparency policy that directs hospitals to make the costs of procedures accessible to the general public.
However, a survey of published charges at hospitals in Louisiana, Arkansas, and Texas and a report of the findings conclude that American patients are nowhere closer to being able to guess the ultimate costs of their healthcare.
“In 2019, Alex Azar, Health and Human Services Secretary for the Trump Administration, said hospital price transparency rules would bring “revolutionary” changes for our healthcare system. The rules would shine the light on the costs of our shadowy system and put the American patient in control,” said David Thompson, lead researcher at ACORN International.
The data collected for the ’“Hospital Pricing Transparency and Its Implementation in Arkansas, Louisiana, and Texas” report, released in March 2022, shows that hospitals fail to follow the feds’ pricing transparency regulations.
“Our team of researchers at ACORN International, Labor Neighborhood Neighbor Training and Research Center, and United Labor Unions Local 100 found American patients are nowhere closer to being able to guess the ultimate costs of their healthcare than they were before the federal requirement.
Hospitals are reporting prices “in wildly different ways, if at all,” with no enforced penalties for non-compliance.”
The Lack of Standardized Prices Allows Hospitals to Charge a Range of Prices For The Same Procedures That Makes No Sense
The data shows patients are still in the dark about their estimated costs. “Transparency for patients remains low. A minority of hospitals in Arkansas (39%), Louisiana (42%) and Texas (30%) have truly accessible price estimation tools,” Thompson confirms.
“Among those, the range of estimates can vary so widely as to make them useless. When an “estimate” for an operation can range between $9,000 and $200,000 at one hospital, how is a patient supposed to be able to make an informed choice?” Thompson says about a procedure at Highland Medical Center in Shreveport.
Prices for an endoscopy at Texas’s Baptist Medical Center in San Antonio offer a striking example of how much different prices for the very same procedure can vary. The minimum negotiated price the hospital agreed to with an insurer for an endoscopy is $614.51. And the maximum is $4,069.19. The cash discount (what an uninsured person is billed) is $15,820.21. The gross price is $21,094.01.
After factoring in all the additional costs and codes, the patient/insurer cost presumably is somewhere in that range.
The report also found that for-profit hospitals’ charges are higher than non-profits and government hospitals in Texas and Arkansas. But in Louisiana, non-profit costs are much closer to for-profits. Texas rates are higher than the three states, followed by Louisiana and Arkansas.
The metro areas with the highest list prices in each state are hospitals in Lake Charles, Longview, Texas, and Fayetteville-Springdale-Rogers areas in Arkansas.
Less Than Half of metro New Orleans Hospitals & Surrounding Parishes’ Hospitals Offer Accessible Pricing Tools.
The New Orleans metro area has 23 hospitals, seven government hospitals, eight non-profits, and eight for-profits. Only 48 percent of hospitals have accessible price comparison tools.
- Accessible comparison tools: Ochsner Medical Center Kenner LLC, Slidell Memorial Hospital, Ochsner Saint Bernard Parish Hospital, Saint James Parish Hospital, Tulane Medical Center, United Medical HealthWest New Orleans, University Medical Center New Orleans, West Jefferson Medical Center, Saint Tammany Parish Hospital, Ochsner St. Charles Parish, and Jennings American Legion Hospital.
- Unreliable or unavailable tools: Ochsner Medical Center Jefferson Highway, River Oaks Hospital, Our Lady of the Lake Southern Surgical Hospital, Saint Charles Surgical Hospital, Ochsner North Shore Extended Care.
- Difficult to access: Avala Hospital’s comparison tool is hard to access because of its complicated excel spreadsheet format.
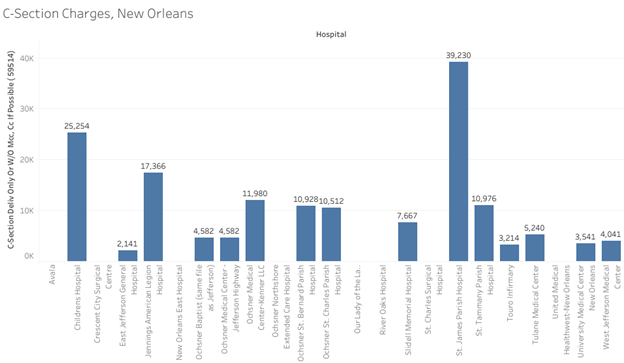
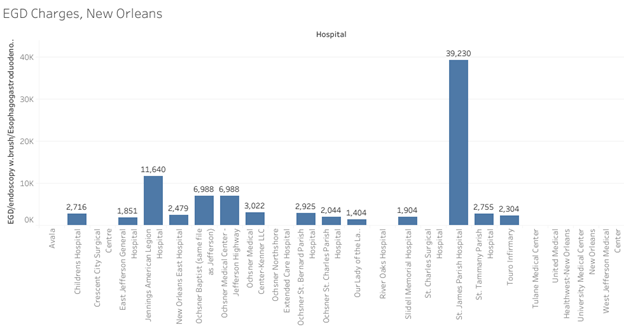
The following graphs offer price comparisons:

There is Light at the End of the Tunnel
Researchers concluded that the government’s price transparency regulation is failing because there are no “meaningful penalties for non-compliance and no standardization” of prices as part of the regulation.
“Moreover, the industry preference for consumer price tools is woefully inadequate even when they “work,” as hospitals do not report estimates within a reasonable range.”
The government and hospitals could both improve the pricing transparency system by requiring a set coding system, plain language descriptions of procedures, requiring insurers to disclose reimbursement data, and instituting significant penalties for hospitals and insurers who are non-compliant.
The Trump administration hinted that it may impose penalties for non-compliance. Still, President Biden’s DHHS and CMS executives have expanded the scope of the previous Administration’s regulations and have added stiff penalties.
Trump’s DHHS pricing transparency rules focused on healthcare consumers’ access to prices before submitting to procedures and competitiveness in the healthcare marketplace.
Related: Fix MAAP Loans for Hospitals
Last July, CMS announced hospital pricing rules to “Increase Price Transparency, Access to Care, Safety & Health Equity” and promote competitive prices for healthcare.
On the same day that it announced the expanded Price Transparency rule, the Biden-Harris Administration’s Department of Health & Human Services announced the “Surprise Billing” rule, which restricts high out-of-pocket costs to consumers from surprise billing and balance billing.
Surprise billing happens when people unknowingly get care from providers outside of their health plan’s network, including emergency and non-emergency care. Medicare and Medicaid prohibit balance billing (when a provider charges a patient the remainder of what their insurance does not pay). This rule will extend similar protections to Americans insured through employer-sponsored and commercial health insurers.
“In accordance with President Biden’s Competition Executive Order, CMS is further strengthening its efforts to increase price transparency, holding hospitals accountable and ensuring consumers have the information they need to make fully informed decisions regarding their health care,” said HHS Secretary Xavier Becerra.
“As President Biden made clear in his executive order promoting competition, a key to price fairness is price transparency,” “No medical entity should be able to throttle competition at the expense of patients. With the proposed rule, we are simply showing hospitals through stiffer penalties: concealing the costs of services and procedures will not be tolerated by this Administration.”
“CMS is committed to addressing significant and persistent inequities in health outcomes in the United States. The proposed rule helps us achieve that by improving data collection to better measure and analyze disparities across programs and policies,” said CMS Administrator Chiquita Brooks-LaSure.
CMS must have received many complaints about the hospital’s lack of pricing transparency because the agency posted a statement on the negative feedback it received.
“And CMS takes seriously concerns it has heard from consumers that hospitals are not making clear, accessible pricing information available online, as they have been required to do since January 1, 2021.”
“CMS plans to increase the penalty for some hospitals that do not comply with Hospital Price Transparency’s final rule. CMS said it would set a minimum civil monetary penalty of $300/day for smaller hospitals with a bed count of 30 or fewer and a fine of $10/bed/day for hospitals with a bed count of more than 30, not to exceed a maximum daily dollar amount of $5,500. Under this approach, for a full calendar year of non-compliance, the minimum total penalty amount would be $109,500 per hospital, and the maximum total penalty amount would be $2,007,500 per hospital.
“Based on information that hospitals have made public this year, there is wide variation in prices – even within the same hospital or the same system, depending on what each insurance plan has negotiated with that hospital. CMS committs to ensuring consumers have the information they need to make fully informed decisions regarding their health care. Since health care prices can cause significant financial burdens for consumers,” according to a statement posted on the CMS website.
Biden’s Administration is Seeking Input from the Public Regarding Health Equity
CMS is seeking input on ways to make reporting of health disparities based on social risk factors and race and ethnicity more comprehensive and actionable.
This includes soliciting comments on the potential collection of data and analysis and reporting of quality measurable results by various demographic data points including, but not limited to, race, Medicare/Medicaid dual-eligible status, disability LGBTQ+, and socioeconomic status.
“CMS is committed to addressing significant and persistent inequities in health outcomes in the United States. The new proposed rule helps us improve data collection to better measure and analyze disparities across programs and policies,” said CMS Administrator Brooks-LaSure.
“We are committed to finding opportunities to meet the health needs of patients and consumers where they are, whether it’s by expanding access to onsite care in their communities, ensuring they have access to clear information about health care costs, or enhancing patient safety.”
CMS vows to make annual improvements to the pricing transparency regulation.
The entire “Hospital Price Transparency and Its Implementation in Arkansas, Louisiana, and Texas Report” is in Social Policy 52.1 Magazine.

